Host: Today, we are speaking with Alice Chang, Ph.D. atCMU Institute of Biochemistry, a leading researcher in cancer metabolism, to explore the complex role of methionine in cancer progression and therapy. Dr. Chang, thank you for joining us.
Dr.: It’s a pleasure to be here.
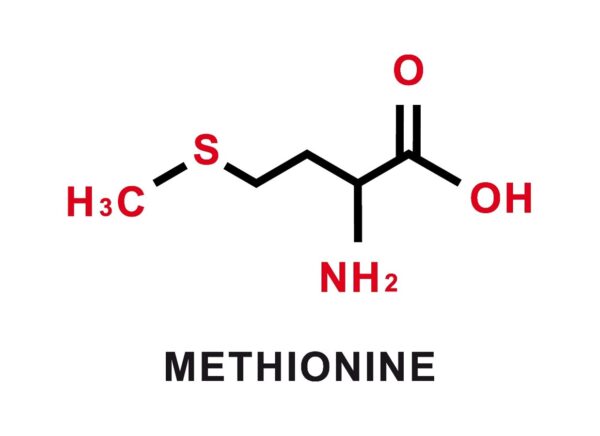
Host: Methionine is an essential amino acid, crucial for many cellular processes. Can you briefly explain its role in cancer?
Dr.: Absolutely. Methionine is critical for a range of cellular functions, including protein synthesis, methylation reactions, and antioxidant defense. For cancer cells, methionine is particularly important for their rapid growth and survival, especially since many cancers have a high demand for this amino acid. On the other hand, methionine also plays a vital role in immune cell functions, including the activation and differentiation of T cells, which are crucial for fighting tumors. So, methionine’s role in cancer is quite paradoxical — it both supports tumor growth and is needed for antitumor immunity.
Host: That sounds like a double-edged sword. How does methionine restriction (MR) impact cancer progression?
Dr.: Methionine restriction (MR) has shown promising results in preclinical studies where it suppresses tumor growth and enhances the effectiveness of various anticancer therapies. This is because cancer cells are often more reliant on methionine than normal cells, so reducing its availability can slow tumor progression. However, T cells, which are key players in the immune response against tumors, also depend on methionine for their activation and function. So, limiting methionine could impair T cell-mediated immunity, reducing the body’s ability to fight tumors effectively, particularly in immunocompetent individuals.
Host: That seems like a significant concern. You’ve mentioned research involving immunocompetent mice. What is MR’s impact on the immune system?
Dr.:Yes, that’s a critical point. It was shown that in mice with healthy immune systems, MR inhibited the activation and expansion of T cells, which exacerbated tumor growth. Essentially, MR suppresses the immune response, making the tumors harder to control. This is a major concern for applying MR as a cancer treatment in patients with intact immune systems, particularly early in cancer progression when immune responses are most important for containing tumor growth. However, in mice with weakened or deficient immune systems — which are often used in cancer studies — MR was beneficial, reducing tumor growth and improving the response to therapies.
Host: So, MR could have a different effect depending on the immune status of the individual?
Dr. Alice Chang, Ph.D.: This is a nuance. In patients with healthy immune responses, MR could impair T cell function, ultimately promoting tumor progression. The effects may likely be very different in patients with compromised immunity. This duality is one of the reasons why methionine restriction as a dietary strategy for cancer treatment remains controversial. It really depends on the tumor stage and the immune status of the patient.
Host: That’s fascinating. Can you expand on the role of the gut microbiota in this process?
Dr.: Yes, the microbiota plays an important role. It was shown that MR affected the gut microbiome, which in turn influenced immune cell function. Specifically, MR led to a deficiency in hydrogen sulfide production by microbiota. Hydrogen sulfide is critical for immune cell survival and activation, so when its production is reduced, the immune system’s ability to fight the tumor is compromised. Interestingly, supplementing methionine reversed this effect, improving antitumor immunity and suppressing tumor growth, partly through microbiota-mediated pathways.
Host: That’s a novel perspective. You also mentioned another research involving cGAS activity in relation to MR. Could you elaborate on that?
Dr.: Yes, cGAS is a sensor of cytosolic DNA, and its activation triggers type I interferon responses that are crucial for antitumor immunity. It is known that MR enhances cGAS activity by preventing its methylation. This methylation normally inhibits cGAS function by sequestering it in chromatin. By blocking methylation, MR allows cGAS to be more active, which boosts antitumor immunity. It suggests that nutrient stress, like methionine deprivation, can activate immune responses through epigenetic changes, offering a potential therapeutic strategy to enhance immunity against tumors.
Host: In light of all these findings, how should methionine be considered in clinical cancer treatment?
Dr.: In clinical settings, methionine should be carefully considered, taking into account both the immune status of the patient and the stage of the tumor. For immunocompromised patients, MR may be a useful adjunct therapy. However, for patients with an intact immune system, especially in the early stages of cancer, MR could hinder the immune system’s ability to fight the tumor.
Host: Dr. Chang, this has been insightful. Thank you for sharing the research with us today.